Learn about HPV as we answer common questions and explore how vaccination can protect children
The bottom line for caregivers
|
Understanding HPV
What is human papillomavirus (HPV)?
HPV is a family of common viruses that live on the skin, including around the mouth, throat and genitals. Human papillomaviruses have been with us for millennia, dating back to early human ancestors and Neanderthals. They spread through close contact, including sexual activity.
Nearly everyone will get HPV at some point in their lives. Many infections will be harmless and are cleared by our immune systems. However, some people don’t clear the virus properly. These ‘persistent infections’ can cause cancer after several years.
Cervical cancer is strongly linked to HPV infection. In fact, more than 95% of cervical cancer cases are caused by HPV. Cervical cancer is most often diagnosed in young women, aged 25 to 35 years. HPV infections can also cause cancer of the vagina, vulva, anus, penis, head and neck, and anogenital warts (warts that that involve the anus and the genitals).
Why does my child need the HPV vaccine?
Cervical cancer is the 4th most common cancer worldwide, causing more than 350,000 deaths each year. The good news is that cervical cancer is one of the few cancers that can be prevented by a simple vaccine. Vaccination can prevent the types of HPV that cause cancer and anogenital warts.
Who is most at risk?
Cervical cancer can be reduced in countries that have highly effective screening and treatment programmes. However, HPV vaccination has the biggest impact in countries that don’t have the resources for screening and treatment programmes.
Cervical screening, to find and treat people with the precursor changes to cancer (cervical pre-cancer), is still important. This is still true, even if you have been vaccinated. The vaccines do not cover every HPV that causes cancer, just the most common. The aim to eradicate cervical cancer globally needs a combination of vaccination, screening and treatment for pre-cancer.
Currently, more than 85% of all cervical cancer deaths occur in low- and middle-income countries. Our data shows that almost all of these could be prevented through routine HPV vaccination, screening and treatment of pre-cancer.
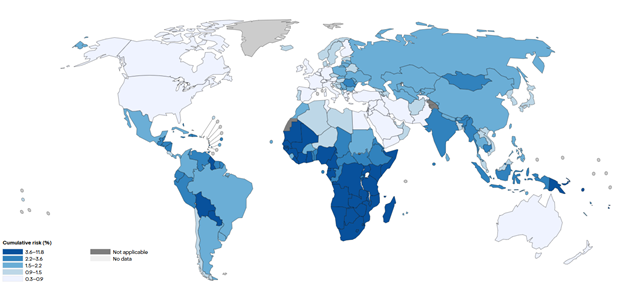
This map shows a woman's risk of developing cervical cancer in her lifetime, based on World Health Organization data from 2022. The lower risk in high-income countries is due to population-wide vaccination and screening programmes.
What’s new?
We wanted more information on long term and rare outcomes of the HPV vaccine that one-off studies can't answer. So, we reviewed two types of studies:
- Population-level studies (real-world data from millions of people)
- Randomized controlled trials (scientific studies comparing vaccinated and unvaccinated groups)
The results were clear; HPV vaccination of young adolescents protects people from cancers and genital warts, with only minor short-term side-effects.
Does the HPV vaccine work?
We looked at 225 studies, including 132 million people across multiple countries. The findings showed that if girls have the HPV vaccination before the age of 16, they have an 80% lower risk of cervical cancer compared with those who were not vaccinated. But how effective the vaccine was depended on the age it was given.
The research also showed the vaccine protected children from anogenital warts and cell changes, which can be a precursor to cancer. However, some HPV-related cancers take even more years to develop. For these cancers the long-term effects of the vaccine are still being studied and the evidence is more limited.
The take home message is that this works. Vaccinating girls and boys protects them from cervical cancer, helping them to lead happy and healthy lives.
Is the HPV vaccine safe?
Our reviews found that some minor reactions such as local pain and swelling were found after HPV vaccination, but there were no serious harmful effects.
On top of this, we looked specifically for evidence about common concerns about HPV vaccines. We thoroughly investigated the top 10 side effects reported on social media, including chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME), complex regional pain syndrome and paralysis. None are linked to the vaccine.
A worry for parents is often whether the HPV vaccine causes infertility. Our review found with high certainty that the HPV vaccine does not cause fertility problems.
However, cervical cancer and its treatments can lead to infertility. For example, people with cervical cancer might receive chemotherapy or radiation, or need surgery to remove their womb. Getting the vaccine and reducing the likelihood of cervical cancer protects fertility.
“If you vaccinate when you're under 16 then there’s an 80% decrease in the number of cervical cancers that we’re seeing. And that’s just amazing that we can do that.” - Dr Jo Morrison, Consultant Gynaecological Oncologist, Somerset NHS Foundation Trust
Getting vaccinated
Why should we give the HPV vaccine at such a young age?
Vaccination is most effective when it is given before children come into contact with HPV, which is normally through close sexual contact. That’s why giving the HPV vaccination to children before they are 16 years old protects them before they are exposed.
Some parents are concerned that giving the HPV vaccine at a young age encourages children towards riskier sexual behaviour or earlier sexual activity. But our review shows no link between HPV vaccination and increased or earlier sexual activity.
Do boys need the HPV vaccine too?
Anyone can get and spread HPV. We know that vaccinating boys protects them from HPV infection and anogenital warts. It could also help to prevent other forms of cancer, although the evidence is less certain. HPV can cause head and neck cancers, as well as penile and anal cancers. As these cancers tend to develop later in life, there has not been enough time since HPV vaccinations were introduced to study the impact on these cancers.
Vaccinating boys also improves ‘herd immunity’, reducing rates of HPV in the overall population and giving better protection to girls too.
How can we get the HPV vaccine?
It is easy to get vaccinated. More than 145 countries have integrated HPV vaccines into routine immunization schedules. In some countries you need to take your children to see a healthcare professional, other countries provide programmes through schools and all you have to do is sign a consent form.
